- About
- Organization
- Organization Overview
- Dean’s Office
- Department of Bioengineering and Therapeutic Sciences
- Department of Clinical Pharmacy
- Department of Pharmaceutical Chemistry
- Quantitative Biosciences Institute
- Org Chart
- Research
- Education
- Patient Care
- People
- News
- Events
Posters tracking beta blocker side effects, antibiotic use, blood thinner adherence take top seminar honors
By David Jacobson / Wed May 22, 2013
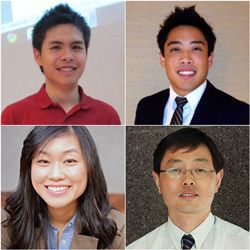
Rifkind award winners (clockwise from upper left) Tony Huynh, PharmD; Alan Chuang, PharmD; Jaekyu Shin, PharmD; Michelle Shen, PharmD.
Studies of whether patients are taking a blood thinner as prescribed, whether antibiotic treatment of cancer patients’ fevers matches guidelines, and whether one form of a leading cardiovascular drug increases the risk for a serious side effect took top honors at the Department of Clinical Pharmacy’s 15th annual Spring Research Seminar.
The poster session, covering a total of 42 projects and highlighting research by UCSF School of Pharmacy student pharmacists, residents, and faculty members, was held on May 6, 2013 on the Parnassus Campus.
Rifkind Award Winners
Winners of the 6th annual Gary Rifkind Spring Research Seminar Awards are:
Student Pharmacist
Alan Chuang, PharmD, and Tony Huynh, PharmD (both class of 2013), for “An ambulatory care program to evaluate patient adherence to the oral anticoagulant: dabigatran.”
Resident
Michelle Shen, PharmD, for “Vancomycin de-escalation in febrile neutropenic patients on the Hematology/Bone Marrow Transplant Service at UCSF Medical Center.”
Junior Faculty
Jaekyu Shin, PharmD7, for “Comparison of the risk of bradycardia between two oral metoprolol formulations.”
The Rifkind awards, $1,000 each, were created to recognize and inspire clinical pharmacy research. They are the gift of Gary Rifkind, PharmD, a UCSF School of Pharmacy alumnus, class of 1960.
Evaluating patient adherence
A study lead-authored by Chuang and Huynh evaluated whether ambulatory patients prescribed the drug dabigatran to prevent blood clots and strokes due to an irregular heartbeat were taking it as directed, also known as adherence.
Unlike the widely used blood thinner warfarin, dabigatran does not require routine lab monitoring. But that benefit can be a double-edged sword, the poster noted, limiting adherence follow-up and education, as provided by a specialty ambulatory clinic such as the UC Davis Medical Center (UCDMC) Anticoagulation Clinic.
The researchers used UCDMC electronic medical records to identify patients prescribed dabigatran during 2012, then followed up with pharmacies to check on supplied quantities and refill pick-up dates. They applied a measure of adherence dubbed Mean Possession Ratio (MPR), which divides the days of total drug supply by the days of the study period.
They found that an adherence problem existed, with more than half of the 155 study patients having access to their prescribed medication less than 80 percent of the time—a common threshold used in adherence studies of medications for chronic conditions requiring twice-a-day dosing.
Chuang, Huynh, et al., conclude that a monitoring program is needed to follow up with patients prescribed dabigatran since poor adherence might affect clinical outcomes. Specifically, they recommend:
- Monitoring renal function, side effects, and dosing
- Determining and addressing barriers to adherence (e.g., affordability)
- Delivering refill reminders by phone
- Providing on-going patient education
Analyzing antibiotic use
Shen’s poster analyzed the use of the antibiotic vancomycin in patients admitted to the UCSF Medical Center hematology/bone marrow transplant service for treatment of blood cancers such as leukemia, lymphoma, and multiple myeloma.
Such malignancies and their treatments often result in neutropenia (low levels of blood cells that fight bacterial infections) and more than 80 percent of these patients develop fevers.
Shen and her co-authors note that the service’s guidelines recommend giving intravenous vancomycin to patients with neutropenia and fever, while also starting tests to determine if, in fact, the fever is caused by a Gram-positive bacteria, which the antibiotic targets. Those guidelines also call for stopping the drug’s use if a blood culture does not reveal such bacteria within 72 hours.
The main goal of Shen’s study was to determine how often the antibiotic was started in the specialty service, how often it was being administered for more than 72 hours and, in the latter cases, what evidence was used to support such continued use.
After reviewing the charts of the 288 adult patients who received vancomycin for neutropenia-associated fevers during the first nine months of 2011, the researchers found that:
- Half of patients were given the antibiotic for more than 72 hours, and nearly 80 percent of them did not have blood work showing Gram-positive bacteria.
- The most common reason given for vancomycin’s continued use was “persistent fever” (40 percent), while nearly as many cases had no documented reason (36 percent).
The project’s findings suggest future directions that include:
- Reiterating the vancomycin use guidelines in staff education
- Requiring documentation of reasons for its extended use
- Further analysis of patient and bacterial outcomes when the antibiotic is used for more or less than 72 hours
Comparing side effect risks
The study by Shin and colleagues examined whether taking one form of a leading high blood pressure and heart disease drug—immediate versus slow release pills—increased the risk of a serious side effect.
The drug, metoprolol, is the most widely prescribed oral beta blocker in the United States. Such medications reduce the binding of stress hormones to cell beta receptors and are used to treat conditions such as hypertension, heart failure, and disturbances in heartbeat rhythm. A potentially serious side effect can occur if the drug causes the heart to beat too slowly (bradycardia).
Shin and his co-authors compared how often patients starting to use either the immediate or slow release versions of metoprolol went to the emergency room or were hospitalized due to drug-related bradycardia. To do this, they analyzed more than five years of records (2004-2009) from California’s Medicaid program, involving nearly 32,000 patients taking the drug.
Based on their analysis, the researchers found that:
- Overall risk of the side effect from either form of metoprolol is low.
- As hypothesized, based on higher peak blood concentrations, the immediate release form, given at the same daily dose as the slow release, increased the risk of slowed heartbeats.
- Even after adjusting for patients’ other medical conditions and the use of other drugs influencing heart rates, those starting on the immediate release form of the drug were 50 percent more likely to suffer serious bradycardia.
Tags
Topics:
Category:
Sites:
School of Pharmacy, Department of Clinical Pharmacy, PharmD Degree Program
About the School: The UCSF School of Pharmacy aims to solve the most pressing health care problems and strives to ensure that each patient receives the safest, most effective treatments. Our discoveries seed the development of novel therapies, and our researchers consistently lead the nation in NIH funding. The School’s doctor of pharmacy (PharmD) degree program, with its unique emphasis on scientific thinking, prepares students to be critical thinkers and leaders in their field.



